Key Topics
- What the surgery involves
- Risks and complications of surgery
- Your preparation for an oesophagectomy
- After an oesophagectomy
What is an oesophagectomy?
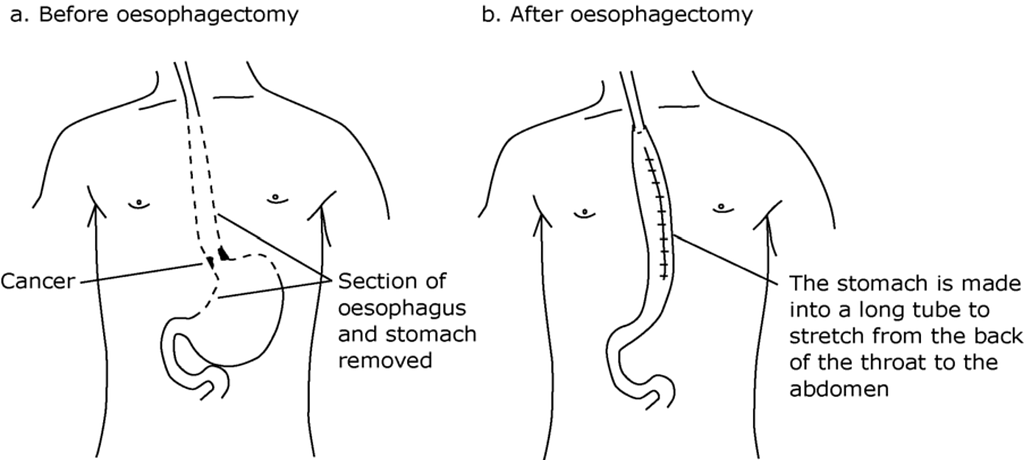
An oesophagectomy involves removing most of the oesophagus (gullet) and part of the stomach with the draining lymph glands (these are small, bean-shaped glands that filter bacteria and disease from the lymph fluid).
A tube is made out of the stomach which is then joined up (known as an anastomosis) to the remainder of the oesophagus in the chest. In order to do this, the Surgeon will make incisions (cuts) in the abdomen and right side of the chest. Sometimes an incision is also made in the left side of the neck.
What does the surgery involves?
There are different ways of carrying out the operation depending on the size and position of the cancer. Your Consultant Surgeon will discuss with you which type of operation is most suitable for you.
In this hospital, most oesophagectomies are performed either entirely or partly by keyhole surgery (laparoscopically) rather than an open operation. In some cases the operation has to be done as an open operation. An oesophagectomy is a major operation and the entire operation can take between 6-8 hours to perform.
You should be aware that there is a small chance (5% or 1 in 20) that the keyhole operation may need to be converted to an open procedure.
Position of wounds
If you would like to know where your operation incisions will be, please ask your Consultant Surgeon.
What are the possible risks and complications?
Before the operation your Surgeon will discuss the risks associated with the operation. The most common complications include the following:
- Chest infection – Chest infection is quite common after an oesophagectomy. About a quarter of patients will require antibiotics for this. A smaller number of patients may have a chest infection that may require spending time on the Critical Care Complex (CCC). If you have chest problems to start with (asthma, chronic obstructive pulmonary disease or smoking-related chest problems) then a chest infection after the operation can be severe and life-threatening. Please note that the incidence of this is significantly higher in smokers (please see the section below on stopping smoking).
- Bleeding – An oesophagectomy can occasionally lead to life threatening bleeding which may require a second operation to stop the bleeding. Some patients may need a blood transfusion. If you have concerns about blood transfusion please let your Surgeon and Anaesthetist know before the operation.
- Anastomotic leak – An anastomosis is a join between the remainder of the oesophagus and the stomach tube that is brought up into the chest. On occasions, the anastomosis doesn’t heal as well as it should and it can leak (5 to 10% chance) – this risk is particularly higher if you are still smoking. This can be life threatening and may require further surgery and a much longer hospital stay.
- Chyle leak – This is a leak of milky fluid due to inadvertent injury to the thoracic duct during surgery. To help the leak heal you will need to follow a fat free diet. More specialist dietary modification may be required which could delay your discharge. If the leak persists despite these measures further surgery may be required.
- Blood clots – Deep vein thrombosis (DVT) or pulmonary embolus (PE). This risk is reduced with injections (see below for more information on this).
- Heart problems – Irregular heart beat (atrial fibrillation), heart attack, heart failure. An irregular heart beat is a common event after an oesophagectomy and is usually treated with medications.
- Feeding tube/jejunostomy complication – If you have a feeding tube inserted there may be increased risk of infection, twist or a leak. This maybe treated with antibiotics or may require another operation.
- Stomach tube necrosis – Breakdown of the new stomach tube tissue. This would need further major surgery. Please note that the incidence of this is significantly higher in smokers.
- Death from the operation – Unfortunately despite our best efforts there is a risk of death with an oesophagectomy. The death rate is less than 1% at the NNUH and this compares favourably with the national average of 5%.
Your preparation for surgery
Your preparation for surgery starts at the point you are told you will be having surgery as part of your treatment and continues on discharge home from hospital after your surgery.
It is absolutely essential to do everything possible to get you home safe and well after an oesophagectomy. As a team we will do our utmost to perform the operation safely and look after you after your surgery. However we need you to adhere to the advice below regarding smoking cessation and cardiovascular exercise which if followed closely can greatly reduce the risk of complications and improve your chance of doing well.
You must STOP smoking.
If you smoke, it is essential to STOP SMOKING NOW.
During the surgery your right lung is deflated for a whole afternoon, so it is essential to have as healthy lungs as possible to reduce the risk of breathing and chest problems after surgery. As above, you have an increased risk of anastomotic leak if you continue to smoke.
Nicotine patches or electronic cigarettes should NOT be used as these can also cause complications. You must adhere to this advice as it can make the difference between life and death.
For help on giving up smoking please contact “Smokefree Norfolk”, the stop smoking service in Norfolk, on 0800 0854 113 or via your GP or health centre. Your Doctor, Practice Nurse or Health Visitor can also give advice to help you stop smoking.
Why is exercise before surgery vitally important?
You need to be as fit as possible before your operation as this will help you to recover more quickly afterwards and prevent life threatening complications. It can also mean that if you develop a complication you are much stronger to get better. Before surgery the fitness of your heart and lungs can be hugely improved by a small amount of exercise each day.
Any form of exercise which raises your heart rate and burns calories is beneficial. This can include the following:
- Everyday activities: walking, heavy housework, gardening.
- Long walks, cycling, dancing.
- Golf, swimming.
How much exercise will you be expected to do?
We recommend that during your chemotherapy (if you are having this) and the weeks before surgery you should try and do the following:
- 30 mins of moderate exercise at least 5 days a week such as brisk walking or cycling at a comfortable pace.
Or
- 20 mins of vigorous exercise 3 times a week such as jogging, swimming or cycling at a fast pace.
And
- Complete strengthening activities on at least 2 days a week.
For more information refer to NHS website www.nhs.uk/live-well/exercise/
It is essential that you maintain a healthy diet leading up to surgery. If you are still struggling with eating or losing weight you must be seen by a dietitian to give advice on diet and assess your need for food supplements. Your Doctor or Nurse Specialist will refer you.
The weeks leading up to surgery
You will receive an appointment to attend the preoperative assessment clinic to be screened for Methicillin Resistant Staph Aureus (MRSA) and to perform investigations such as heart rate, blood pressure and weight. You may have blood tests, a chest X-ray, and an electrocardiogram (heart test) and you will be seen by an Anaesthetist.
You will be given information about what to bring into hospital.
Please bring a list of all your current medication when you attend the clinic.
You may be given a medicine to take the night before and the morning of the operation to reduce the amount of acid in your stomach.
The Anaesthetist will see you to assess you and discuss the surgery and anaesthetic with you.
Some pre-operative assessments may be performed via telephone consultation – you will be informed of which style appointment you will have when the appointment date is confirmed with you. Please have a list of your current medication available for this pre-operative assessment telephone call.
A cardiopulmonary exercise test lets your Doctor see how your lungs, heart and muscles react together when you exercise. It involves you cycling on an exercise bike while we will measure how much air you breathe, how much oxygen you need, and how fast and efficiently your heart beats when you exercise.
To measure the amount of air that you breathe, you will need to wear a soft, comfortable facemask covering your mouth and nose. An ECG (electrocardiogram) will look at the rhythm and rate of your heart, a blood pressure cuff will measure your blood pressure throughout the test and a small peg on your finger will measure how much oxygen is in your blood.
What will happen on the day of surgery?
You will either come in the day before or on the day of surgery depending on your Surgeon’s preference. If you are admitted on the day of surgery you will be asked to attend the Same Day Admissions Unit (SDAU), where you will be taken to theatre. When you attend please bring in all your current medication.
The operation
The operation is performed under general anaesthetic (you will be asleep whilst the operation is performed). The operation takes 6-8 hours.
Before the operation starts the Anaesthetist will spend time placing a spinal/epidural injection as well as starting the general anaesthetic.
While you are asleep, you will also have other tubes connected to you: a urinary catheter to drain urine, a tube down the nose to drain the stomach, and tubes in the abdomen and chest (see below).
After the operation, your Surgeon will telephone your next of kin to explain how the surgery went.
After the operation
What to expect whilst you are in hospital
Most people are in hospital for 5-10 days. If there are complications, your stay may be longer. After the operation it is routine for patients having surgery for cancer of the oesophagus to spend the first few days in the Critical Care Complex (CCC) to be monitored closely until stable enough to return to the ward.
After an oesophagectomy you will experience some discomfort. This is usually controlled by the epidural method of pain relief. This involves inserting a thin plastic tube in your back just before the operation. It is attached to a pump to give you continuous pain relieving medication until you are ready to take tablets. The Anaesthetist will discuss this with you before the operation.
If you are having minimally invasive oesophagectomy (MIO keyhole surgery) you will have a spinal block for pain then a PCA (patient controlled analgesia) – where you press a button to get the pain killer when you need it.
It is important to make sure you have adequate pain relief so you can move around and cough to prevent complications. The Physiotherapists will work closely with you to help your lungs recover and prevent breathing complications. This is the most important part of your recovery process and it is very important that you follow their instructions and allow them to help you get going. The sooner you are able to stand and then walk (with help) the better for your recovery.
You will have one or usually two drains coming out of the chest. The drains are placed to allow fluid and air to drain from the chest. They are removed once the fluid stops draining – this is straightforward and easily done at the bedside.
You will have a urinary catheter placed into your bladder to monitor your urine output initially, and it is removed when you are able to walk to the toilet (after the epidural has come out). You will also have a small tube down your nose to drain any digestive fluids until the join (anastomosis) heals.
You will be allowed a water to wet your mouth every hour directly after surgery.
You will be advised when to start eating; it usually takes 3-4 days. You may require an endoscopy or a barium swallow (an X-ray test that requires you to drink a liquid to show how it drains into the gut) before your Consultant is happy for you to start eating.
The Dietitian will see you regularly before and after your surgery to advise you about your diet and give you advice about meals. Your appetite will take a while to return. It is important to understand that you will not be able to eat large meals and will need to eat small and frequent meals. It can take a while to get used to this new way of eating.
Physiotherapy after surgery
The Physiotherapist will see you the morning after your operation and ensure you are able to breathe deeply and cough effectively. They or the nursing staff will assist you out of bed and to begin to mobilise. You will continue to be seen by the Physiotherapist daily to help you progress your exercise and walking until you are fully independent and able to continue by yourself.
Walking, deep breathing exercises and coughing
Breathing exercises are important following surgery and can help prevent chest infections and other lung problems. You should start them as soon as you wake up from surgery and practise them every half an hour.
- Sit in a comfortable upright position with your shoulders relaxed.
- Take a slow deep breath in (through the nose if possible) filling the bottom of your lungs.
- Hold for 3 seconds and then relax and breathe out gently through your mouth.
- Repeat 3 more times and then rest (more than this may make you feel dizzy or light headed).
- Following deep breathing exercises it is important to cough and clear any phlegm that you produce.
Coughing may be more comfortable and effective if you either sit forward or bend your knees and support your wound with your hands or a folded towel.
If deep breathing or coughing is too painful then please tell your Nurse.
Leg exercises
When in bed:

- Point your toes and rotate your feet in a circular motion
- Repeat 10 times on each leg

- Tighten your thigh muscles by pushing the backs of your knees down against the bed, hold for 5 seconds
- Repeat 10 times on each leg

- Bend and straighten each leg 10 times
- Keep your foot close to the bed but do not drag your heel on the sheet as this can make your heel sore
When in the chair:

- Straighten one knee, pull toes up and hold for 5 seconds
- Repeat 10 times
- Repeat on the other side

- March your legs in sitting, lifting each foot in turn
- Aim to complete for 3 minutes
Walking
Walking will start on the first day after your operation. Drips and drains move with you and will not stop you getting out of bed and walking. The physiotherapy and nursing staff will help you until you can walk by yourself safely. Once able to walk independently you will be responsible for walking regularly. We will aim for you to be walking 5 laps around the ward 4 times a day on day 4 after your surgery. The more you do the better it is for you.
Histology and chances of cure
The histology report (the review of the cancer tissue removed) takes approximately 2 weeks to become available. The success of the surgery in terms of cure is dependent upon how early the cancer has been detected. The removed part of the oesophagus or stomach is sent to the laboratory and examined to identify the stage of the cancer. The stage of cancer depends on how far the cancer has grown out from the wall of the oesophagus and stomach, into the surrounding lymph nodes. Sometimes more treatment is needed after surgery – this may involve radiotherapy and/or chemotherapy – to help to reduce a recurrence of the cancer. Your Consultant will discuss this with you after the operation if it is appropriate.
Tablets and drugs
Your usual tablets and drugs will be given to you when you are drinking properly. If they are important tablets, we can give them either down a feeding tube or intravenously (through a vein).
Dalteparin injections are routinely given through a tiny needle once a day to minimise the risk of a blood clot in the legs (DVT or deep vein thrombosis) and lungs (pulmonary embolism). This should be continued for 28 days after the operation and this will usually mean getting yourself or a family member to give it once you are home. The ward nurses will support you in learning how to use these injections before you are discharged.
What to expect when you get home
The following information will hopefully answer a number of common questions that many patients have about their care after an operation of the oesophagus.
For the first 2 weeks after surgery your Consultant may instruct you to remain on a liquid diet before moving on to a sloppy/soft diet. You should progress to eating most foods about 4-6 weeks after surgery but be guided by your Consultant, Dietitian and Nurse Specialist about when to progress to normal diet.
Please refer to the diet sheet provided by the Dietitians for suggested meals and snack ideas.
Amount of food
After the operation you will need to significantly reduce the amount of food and drink consumed at one time. This change will be for life. You should eat what you like but you will find that you become fuller much quicker than before as the new stomach is now smaller.
You should have been given a diet sheet by the ward Dietitian prior to going home. Often people do not feel very hungry after oesophageal surgery, but it is important that you do try and eat as much as you can. You will probably require more than 3 meals a day. It is a good idea to have several snacks in between meals to make up for the food that you can’t eat during main meals as you feel too full. Over time this will get better.
Main points of advice are as follows:
- Do not drink before or during a meal.
- Use a small plate for your main meals.
- Wait at least 30 minutes after a meal before having a desert.
- As soon as you feel full – stop eating and drinking.
- Walk around after a meal to help it move down.
- Always sit upright when eating.
Altered sensations when eating
It is common after this operation to feel there is a ‘lump’ in your throat area when you swallow. This is a normal sensation to feel in the first 4-6 weeks. You will need to try and ignore it and keep swallowing as usual. If, however, you feel the food is sticking or there is a restriction in food going down, please contact your Specialist Nurse or Consultant for advice.
This may be a sign that the anastomosis has narrowed slightly requiring a gastroscopy to stretch it back. If this is needed it is a straightforward procedure which takes about 10-15 minutes and is done as a day case. For contact details please see below.
Appetite
It is common to have no or very little appetite after surgery. It may be difficult for you and your family/carers to cope with this. You may not feel like eating anything that is prepared for you and/or will not enjoy the taste of food. Not wanting to eat can cause a lot of stress and tension between you and your family as they worry about how you will recover if you do not eat.
Remember to keep to small and frequent portions: you will not progress if you try to eat larger meals. The best way to recover and gain weight is to eat 4-6 small meals a day and have regular snacks. It takes several weeks before your appetite returns. Appetite and taste will improve after about 3 months but you may not regain the same level of appetite as you had before surgery.
Taste
After an oesophagectomy it is normal for people’s taste to change. We do not know what causes this but you will find that some foods you previously liked now taste bad. Similarly some foods you didn’t like before can suddenly become tasty!
It is quite common for some people to experience some reflux of stomach contents into the mouth after an oesophagectomy. This happens because the new stomach is closer to the throat and the valve that used to prevent stomach contents coming back up into the oesophagus has been removed.
Often it is a problem at night or when lying flat. Using extra pillows at night to raise your head may help to reduce this problem. Again, eating frequent small meals and snacks may help.
Main points of advice to avoid reflux:
- Take the anti-acid medication at night.
- Avoid drinking or eating for at least 1- 2 hours before you go to bed.
- Avoid lying flat or leaning over within ½ hr after eating or drinking.
- Remember to eat and drink small portions and frequently.
If reflux is a persistent problem, discuss this with your Nurse Specialist or Consultant.
“Dumping syndrome” is a problem that can occur after oesophageal surgery. The symptoms usually include a feeling of faintness or dizziness, which can occur immediately after eating or within a couple of hours afterwards. The faintness is often accompanied by feeling sweaty and sometimes palpitations, nausea, sickness and diarrhoea.
There are two main reasons for this. Firstly, after a meal food can move too quickly into the intestine and by doing so draw a lot of water into the gut. This
causes a drop in blood pressure.
The more common form of dumping syndrome comes on a little while after eating and again is due to food passing too quickly into the small bowel. This causes sugar to be absorbed very rapidly and as a result the body reacts to this by releasing large amounts of the hormone insulin. This insulin then causes your blood sugar to drop below normal levels. When your blood sugar does become very low you can feel very faint and in very severe circumstances can pass out.
Dumping syndrome is very common but can be reduced by the following:
- Reducing the amount of sugary foods that you eat.
- Eating slowly and take your time over your meals.
- Eating smaller meals but more often.
- Adding a bit of fibre in your diet and increasing the fat content of your food to replace the calories from sugars.
- Avoid very liquid food such as soups.
- It is always worthwhile having a couple of sweets e.g. Lucozade/Dextrose energy tablets/jelly babies in your pocket if you do start to feel faint after you have eaten. One of these will help raise your blood sugar again.
- If none of the above helps, there is medication available that can be tried, which can dampen the sudden rise in insulin levels. You Nurse can advise you.
Diarrhoea is quite common after oesophageal surgery. Part of the operation to remove the oesophagus or stomach involves cutting a nerve called the vagus
nerve. (The nerve is stuck to the side of the oesophagus and the side of the stomach. It is not possible to avoid doing this.) As a result of cutting this a few people can get quite bad diarrhoea. The diarrhoea can be very watery. It is a very annoying symptom to have and it can be quite difficult to treat.
The first line of treatment to try is obviously anti-diarrhoea medicine, which you can buy over the counter, such as Imodium. If this does not help you need to speak to your Consultant or your Specialist Nurse who can advise on other medication.
After an oesophagectomy some people develop a dry cough which can be persistent and cause you to feel sick and regurgitate. Try to keep your throat moist, suck a sweet or try codeine linctus syrup, which will suppress it. You can obtain this through your GP. Also try not to talk too much as this can exacerbate it.
All patients will lose weight after major oesophageal surgery – this is usually about one and a half stone over the first three months. After this your weight should improve slowly. You shouldn’t lose weight after 6 months; if you are losing weight fairly rapidly please let your Consultant or Nurse Specialist know and we will organise an early appointment.
Exercise when you get home
The best exercise after surgery is walking. We advise that you continue to take regular walks and increase the distance that you walk every day. Keep doing your walks for the first 3 months after the operation – there is a risk of DVT (blood clots) in that time. It is important to avoid heavy lifting and strenuous exercise for the first 8 weeks.
Go for a walk every day, even if it is only for a few yards/metres. Try and walk a little further each day. As you exercise, even very gently, the body recovers quicker.
Most people have some swelling of their ankles and legs after major surgery. This is normal and should improve with gentle exercise, regular meals and time.
Returning to normal activities
You should be able to go back to work after three or four months, though take the advice of your Doctor.
Driving is possible after about 2-4 weeks at home if you feel comfortable with doing an emergency stop.
Clinic appointments
You will receive a telephone call from your nurse specialist within a week of discharge, then at 4, 8 and 12 weeks and additional telephone support as required. Please contact the nurse outside of these dates if you have any questions or concerns.
You will normally be seen in clinic at 2 weeks after and again at 4-8 weeks after the operation in clinic to check your wounds and to see how well you are getting on. It is usual to have another blood test at this appointment.
If you have any questions about the surgery and further treatment, then this appointment is the time to ask.
If you are having a lot of problems with eating, you should let us know prior to the clinic appointment.
Remember that your GP will be aware that you have had an oesophageal operation but may not know the full story so if you have any concerns please contact either your Consultant or Upper GI Nurse Specialist.
After the first post-op clinic appointment you will normally be seen at 3-6 months after surgery and then at regular intervals thereafter.
Vitamins
Take multi-vitamin supplements with iron after getting home. You can buy these from any supermarket or pharmacy.
Holidays
Providing you are eating OK and your weight is stable it is possible to go on holiday within 2 weeks of getting home. However, long-haul flights are not recommended in the first 3 months. If you are planning a long holiday let us know and we will fit your clinic appointments around the dates. You should check your travel insurance if you are flying in the first 3 months after your surgery.
Feelings and relationships after a major operation – please also refer to the ‘Coping with stress’ section below
After a major operation, it is usual for people to feel low in mood. This may be related to a number of factors such as lack of energy, poor appetite and a general feeling of frustration.
It is important to remember that it can take up to 3-6 months until you feel you have regained some strength and energy. It may be helpful to set small goals to achieve in the first few weeks after surgery rather than expecting to resume normal daily activities, which you may find you are not be able to do, leading to more disappointment and frustration.
Some people experience similar emotions after surgery to those felt at the time of diagnosis (e.g. anger, tearfulness) because of the impact that an operation can have temporarily on jobs, hobbies and relationships.
It can be difficult to talk to loved ones and explain our feelings or we often assume that they understand how we are feeling. Sometimes it seems easier to keep thoughts locked up but this can be difficult for family and friends. By sharing how you feel, you and those close to you are more likely to be able to support each other during stressful times in your recovery.
It is not uncommon for major surgery to cause a temporary drop in libido. Again, this is often due to lack of energy and physical strength. Try to talk openly with your partner about your feelings. Remember closeness and sexual pleasure can be shown in a number of ways, not just by the act of sex.
You should be able to resume sexual activity as soon as you feel physically able to.
Bed wedge/anti-reflux pillows
The Oesophageal Patients Association (OPA) has teamed up with Putman Pillows to provide their standard bed wedge acid reflux pillow at an approximate price of £27.
To take advantage of this offer please call or email the OPA first and they will give you a discount code.
Call on 0121 704 9860 or email: [email protected]
Readmissions
On occasion, even after getting home, you may develop a complication such as a chest infection requiring admission to a hospital. Your GP may admit you to a different hospital or a different department within the NNUH.
If this were to happen, please ask the team who are looking after you at the hospital to contact the Upper GI team at NNUH and please contact your Upper GI nurse specialist at the NNUH when you are home again so that we are aware of what is happening, where you are and what treatment is being offered. We will like to continue to be involved in your care, as often other hospitals are not familiar with oesophagectomy problems.
You will find contact telephone numbers at the end of this leaflet.
Stress, anxiety and depression (CLICK to expand)
We will all experience stress at some point during our life. You should not aim to ‘cure’ yourself of stress but rather to control it.
Stress may be caused by daily responsibilities and routine events, as well as unexpected events, such as a trauma or illness. It is the body’s reaction to a change that requires a physical, mental or emotional adjustment or response.
Think of it like blood pressure: we all have it, but if it is too high, you have to do something about it. It is the same with stress.
A certain amount of stress is normal when you or a family member has cancer. But some people may be affected more than others, affecting their ability to cope.
When people feel that they are unable to manage or control changes caused by cancer or normal life activities, they often feel distressed.
People cope with stress in many different ways and each have their own ways to deal with it. Before you can develop a strategy to cope with stress, you must first identify the signs and symptoms.
The most common form of stress is a mix of anxiety (tension, nerves) and depression (feeling flat, sad). It often comes with sleep problems, panic feelings and anger.
Signs of stress vary from person to person but some of the most common ones you may recognise are:
Tiredness and/or lack of energy.
- Sleeping or eating too much or too little.
- Feeling on edge; worrying too much or worrying about worrying; struggling to switch off; waiting for the worst to happen.
- Feelings of panic.
- Feeling angry or irritable.
- Have poor concentration.
- Feel worthless, guilty or hopeless.
- Brooding on the past.
- Tearfulness.
Once stress takes hold you may notice:
- Your self-confidence dropping.
- That you become more self-conscious.
- That you feel threat from all sides.
- That you doubt your ability to cope.
- You can’t stop your mind racing.
- Worry/brooding becomes second nature.
- Your body reacts easily.
- You feel your back is against the wall.
- You avoid / withdraw.
- You feel irritable about things which wouldn’t have concerned you before.
Managing your stress with unhealthy behaviours such as smoking or drinking alcohol or becoming inactive can be unhelpful to your quality of life.
Caffeine is a stimulant that affects the central nervous system. The effects of too much caffeine can be very similar to those of stress.
People who use effective coping strategies to deal with stress, such as relaxation and stress management techniques, have been shown to have lower levels of depression, anxiety, and symptoms related to their cancer and its treatment.
Although there is no strong evidence that stress directly affects cancer outcomes, some research suggests that patients can develop a sense of helplessness or hopelessness when stress becomes overwhelming.
First step:
- First you need to acknowledge that you are feeling stressed.
- Take a minute to consider how stress affects you?
- What happens to you when you feel stressed?
There is nothing magical about the way you control stress. Once you have identified the way you cope with stress and started to make healthy changes to the way you respond to it, you can control it more.
What you can do when you feel stressed
Some coping strategies for stress
- Learn relaxation and/or meditation techniques. Relaxation training can also be effective in reducing anxiety and nausea and vomiting, before and after chemotherapy.
- Whilst we may feel we know how to relax, it is important to be taught a way of effective relaxation. The standard procedure is to clench and unclench muscles so they can get used to the processes of tension and relaxation.
Breathing retraining
This is a quick method to use to calm your body. Sit in a comfy chair and relax as much as you can.
- Take a slow normal breath (not a deep breath) and think “1” to yourself.
- As you breathe out, think “relax”.
- Breathe in again and think “2”.
- Breathe out and think “relax”.
- Keep doing this up to 10. When you reach 10, reverse and start back down to 1.
Try to put all else out of your mind. It may help to see the numbers and the word ‘relax’ in your mind’s eye.
Don’t be put off if you can’t master this technique straight away.
You can boost the benefits of this by breathing from the diaphragm:
- Place one hand on your chest and the other over your belly button.
- As you breathe in, the hand on your stomach should be pushed out while the hand on your chest should not move. As you breathe out, your stomach should pull in. Your chest should not move.
- To help, breathe in through your nose, purse your lips and breathe out slowly through your mouth. If you are a chest breather, you may find this difficult at first.
- If you can’t get the hang of this, lie on your back on the floor and practise as it is easier to do this in this position.
Put these two exercises together and do them twice a day. Once you get good at them, practice them at work, on the bus, while watching TV etc…
The aim is to be able to do this no matter where you are. No-one will notice you doing them.
Ways to cope
Pick the ones that best meet your needs:
- Reduce your worry. Ask yourself if worrying makes anything more certain or predictable. Will worrying change the outcome of what happens? Are you focusing on the worst case scenarios? Try to stay focused on the present rather than dwelling on the past or worrying about the future.
- Plan one daily goal. This can be a very small goal. It will help you to have things to aim towards. Set priorities – if you could only do one thing, what would it be? Be realistic about what you can achieve. Don’t take on too much.
- Previous experience. If you feel that you are in a mess, ask yourself if you have been in a similar mess before. How did you deal with it? If what you did worked, try it again. If it didn’t, what could you do differently this time?
- Exercise and participate in enjoyable activities to help reduce your stress. You may be feeling physically too tired to do very much exercise but consider small enjoyable activities you can schedule into your daily routine.
- Maintain a healthy lifestyle. This can improve your energy level. Eating a healthy diet consisting of a variety of foods and getting adequate rest may help you manage the stress and fatigue of the cancer and its treatment.
- Time management. Plan your time, doing one thing at a time and allowing regular breaks. Write a list of all the things you need to do and categorise them into must do’s and should do’s. Drop tasks that are not truly necessary to the bottom of the list or eliminate them entirely.
- Learn to accept help. Often friends and family can run errands, provide transportation, prepare meals and help you with household chores.
- Use problem solving to help you cope with cancer, its treatment and side effects, to increase feelings of control over the disease. When faced with a difficult decision, list the pros and cons for each choice.
- Keep informed about your cancer and remain a fully involved participant in your treatment.Education about medical procedures can help reduce anxiety.
- Social support. You may well feel isolated if you withdraw from your friends and family. Try to gain strength from each other. Communication can help reduce anxiety and the fear that cancer can cause.
- Group support. Other cancer survivors can share their experiences and give you insight into what you can expect during treatment.
- Consider counselling or psychological therapy if you feel that it is getting on top of you and you do not feel able to cope.
- Medication. Antidepressants can be very helpful and support you to cope better with life when you are depressed or anxious. It can also help with some of the physical symptoms. But an antidepressant is unlikely to solve all your problems. You may need to look at other ways to feel better. Once you are feeling a little better, you can look at other things that might be helpful.
Useful contacts for further information
See link to our linked organisations page.
Your points of contact
Upper Gastrointestinal Nurse Specialists (Monday-Friday 9am-5pm)
Angela Longe and Tamara Taylor Tel: 01603 288865
Surgeons: (Monday-Friday 9am-5pm)
Mr Michael Lewis FRCS Tel: 01603 287583
Mr Bhaskar Kumar FRCS Tel: 01603 286418
Ms Loveena Sreedharan FRCS Tel: 01603 287367
Mr Nick Penney FRCS Tel: 01603 286418
Mr Suheelan Kulasegaran Tel: 01603 286418
* In an emergency please contact your GP or 999.